Important technological and medical advances, along with the sophistication and the miniaturization of the equipment used have led to the use of Endoscopy in Gynaecology & Obstetrics. Endoscopy has many applications in modern gynaecology and the list is growing every year. Gynaecological endoscopy is a surgical discipline that uses optical instruments specially designed to help diagnose gynaecological disorders and pathologies such as some infertility problems, small vaginal haemorrhages or endometrial polyps among others. The invention of these tiny devices that enable doctors to operate inside the body without the need for open surgery has greatly improved the conditions of patients.
In Gynaecology, endoscopic surgery is probably the most significant advancement in surgical practice. It is being increasingly favoured over the abdominal approach because of its well recognized advantages like minimal trauma, superb visualization, low incidence of complications, reduction of adhesions, shorter hospital stay, rapid recovery and aesthetically pleasing results with least amount of scarring. Endoscopy has secured a firm place in the management of patients with infertility and endoscopic surgical techniques will develop rapidly in the near future to serve the various needs of female patients.
There are three types of endoscopic surgery in obstetrics and gynaecology: laparoscopy; hysteroscopy; and salpingoscopy.
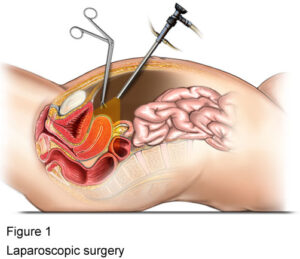
Laparoscopy – With the advances in technology, laparoscopic surgery is rapidly and progressively replacing conventional surgery except for the most difficult cases. Diagnostic laparoscopy is an invaluable tool for assessing patients with chronic pelvic pain, infertility, adhesions and endometriosis, and an adjunct in grading of gynaecological cancers. The excellent visualization of the peritoneal cavity not only aids in diagnosis, but also allows for an accurate assessment of the severity of these conditions. The laparoscopic approach is now the preferred method for the treatment of myoma uteri, ovarian tumours, ectopic pregnancy, infertility, endometriosis and inflammatory masses.
Hysteroscopy – Hysteroscopy has proven to be invaluable in assessing patients with abnormal uterine bleeding, postmenopausal bleeding, infertility and recurrent pregnancy loss. During hysteroscopy the uterine cavity is dilated with liquid and then a resectoscope or hysterofiberscope is used. The development of hysteroscopes with operating channels and instruments such as scissors, biopsy forceps, snares and electrosurgical operating devices such as ball and loop electrodes allow many operative procedures to be performed hysteroscopically. The main indications for hysteroscopic surgery are submucous myoma uteri, uterine anomalies, and Asherman syndrome. Female sterilization can also be performed hysteroscopically with the use of various mechanical occlusive devices or plugs (e.g. Essure).
Salpingoscopy – Salpingoscopy, as a pre-operative diagnostic tool is useful in examining the tubal cavity and a potent tool for tubal recanalization. Salpingoscopy technique allows the direct evaluation of the ampullary tubal mucosa at the time of laparoscopy. The status of the tubal mucosa is the best prognostic factor when evaluating patients with tubal infertility. In the Salpingoscopy procedure a fiberoptic endoscope – salpingoscope is inserted through the cervical canal so the uterus and fallopian tubes can be visualized directly. This can then be used to diagnose and treat obstructions, adhesions or other diseases and conditions. Salpingoscopy, has allowed the improved selection of patients who are candidates for tubal surgery.
For enquiries and online appointments, send a message to www.KJKHospital.com/contact or you can call 0471-2544080, 2544706





